Breaking Out? It Might Be Fungal Acne — Here’s What to Know
2 June, 2025

by Jenna Curcio
Let’s talk about something a little less mainstream and way more common than you’d think: fungal acne.
If you’ve been dealing with clusters of tiny, itchy bumps (especially on your forehead, chest, or back), and nothing seems to help — there’s a solid chance you’re not actually breaking out. You could be dealing with fungal folliculitis, a skin condition caused by — you guessed it— yeast overgrowth, not bacteria.
And that matters. Because if you treat fungal acne like regular acne, it’ll stick around. But once you know what you’re dealing with? That’s a breakthrough moment.
But For Real, What Is Fungal Acne?
First off, fungal acne isn’t really acne. It’s a type of folliculitis — inflammation of the hair follicles — caused by an overgrowth of Malassezia yeast. That yeast lives on everyone’s skin (it’s normal!), but when things get out of balance, it can overgrow and clog up your follicles. Result: itchy, rash-like bumps that don’t respond to typical acne treatments.
How to tell it apart:
-
Fungal acne = tiny, uniform, itchy bumps. Often shows up on your chest, back, shoulders, or forehead.
-
Regular acne = inflamed pimples of different sizes, usually from oil, bacteria, and clogged pores.
Recognizing this difference can seriously empower your skincare routine. The more clarity you have on what’s happening, the better your choices get.
What Causes Yeast Overgrowth?
Short answer: your skin’s balance gets thrown off. Yeast throws a party. Your follicles aren’t thrilled.
Common triggers for fungal acne:
-
Excess heat or sweating
-
Occlusive skincare (hello, heavy oil-based products)
-
Wearing tight or unbreathable clothes
-
Antibiotics or hormonal shifts that mess with your microbiome
-
Diets high in sugar or refined carbs
Basically, it’s a team effort between internal and external factors.
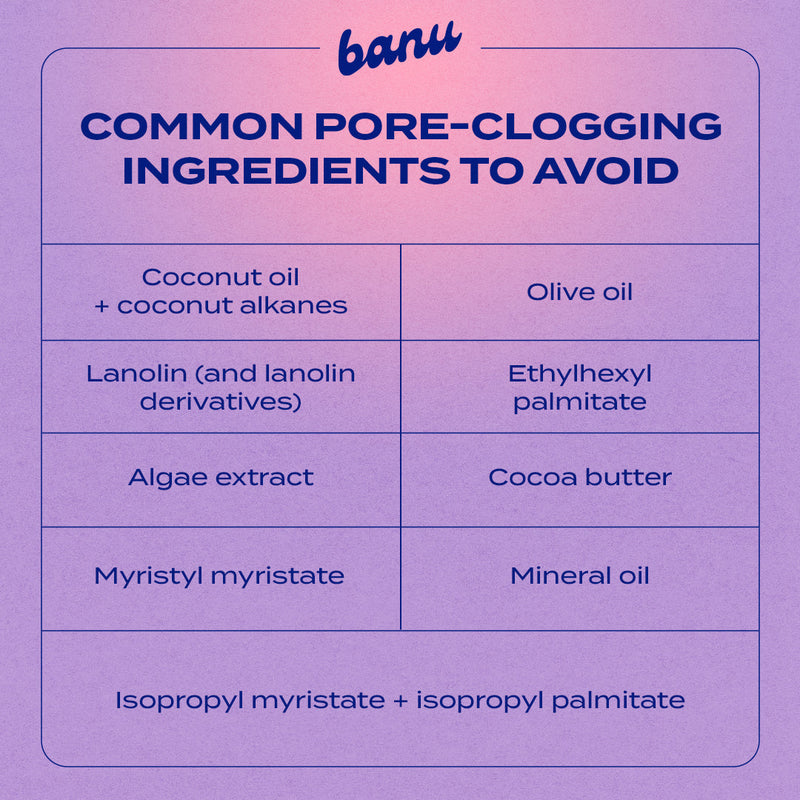
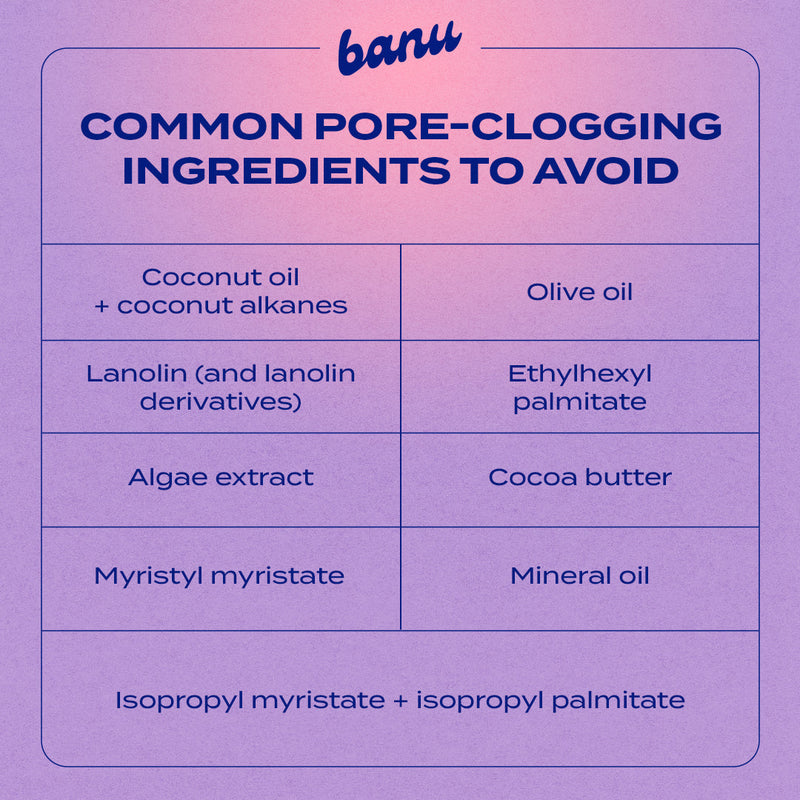
And here’s the thing: not all skincare is fungal-acne friendly. A lot of products contain oils, esters, or fatty acids that feed Malassezia. That’s why banu’s full line is made without fungal acne triggers — on purpose.
How to Treat Fungal Acne
Here are the basics.
-
Stick to Fungal-Safe Formulas
Avoid ingredients that feed yeast (like coconut oil, esters, and fermented extracts). Instead, go for gentle, non-comedogenic basics that keep your skin clear and balanced. -
Bring In Antifungal Helpers
You don’t need to go full Rx unless a derm tells you to, but ingredients like sulfur, zinc pyrithione (yep, even in dandruff shampoo), and diluted tea tree oil can help calm bumps. -
Keep Things Clean + Dry
Fungal acne thrives in heat and sweat. So:
– Shower post-workout
– Wear breathable fabrics
– Wash your gym clothes often
– Avoid sleeping in makeup or heavy creams
When to See a Derm
If your skin’s still flaring after a few weeks of targeted care, check in with a derm. They can confirm if it’s fungal folliculitis — and help fast-track real results.
The Bottom Line
Fungal acne’s annoying, but it doesn’t have to be a whole thing. A few small changes — smarter products, cleaner habits — can make a big difference. You’ve got this <3

Author
Jenna Curcio
Ciao, I’m Jenna :) I’m a writer and brand strategist with 6+ years of experience telling stories in the beauty world — both professionally and personally. After years of dealing with acne, I know how overwhelming and emotional the skincare journey can be. I’m here to make it feel a little less confusing and a lot more human.
The starting lineup
More Reading For You
-
 read more
read moreHoliday Breakouts Are Predictable — Here's the Data Behind Why and What to Do
There's a kind of breakout that shows up around the holidays that just feels different. Not intense. Your skin isn't spiraling — it's just not bouncing back the way it normally does. That usually means something shifted — sleep got shorter, travel picked up, or stress crept in or even your products got heavier. When enough of that overlaps, skin reacts. And once you see that pattern, it gets a lot easier to figure out what actually helps.
-
 read more
read moreAcne & Mental Health: The Overlooked Connection
Image Credit: Instagram Acne can make people feel self-conscious — when you get a breakout it can totally change how you feel about being around people. Acne can make you feel different when you are in a room, with others. We do not talk about this enough. Our skin and mental health are really connected. They are not two things that we struggle with they are actually connected in a big way. When we have acne it can affect how we feel inside.. How we feel inside can also affect our skin. Our skin and mental health kind of work together and one can change the other even if it happens slowly over time. Our skin and mental health are connected in a way that's, like a circle, where one thing affects the other and then that thing affects the first thing again like our skin and mental health. Living with acne really affects how you go about your life. It makes you think about how you look all the time. You become more careful when you are, around people. You start to notice all the things that're wrong with your body. This is very tiring. When your skin is clear you still worry that acne will come back. You are always waiting for the time you get a pimple. Acne makes you feel like this all the time. The stress that people feel is not something that is, in their mind. The stress is also something that they can feel in their body. When you get really stressed out your cortisol levels go up. Cortisol is a deal for your skin because it affects how inflamed it gets how much oil it produces and how fast it heals. So basically the stress that acne gives you can actually make your skin take longer to get better. It is not because you are doing anything but because your body is just reacting to the stress in the only way it can. Your skin and acne are really sensitive, to cortisol. That is why it is so important to think about cortisol when you think about acne. This is the point where the loop really gets tighter. The loop is getting smaller and smaller it is really tightening up now the loop is becoming very tight. Breakouts cause people a lot of stress. This stress then makes the breakouts even worse. Sometimes people are advised to calm down as if being calm was something you could easily do.. When your skin is being really stubborn it is not that easy to relax. Breakouts make people feel really stressed. This stress makes the breakouts worse. What people often forget is that this problem is not about being strong willed or thinking thoughts. It is about how much stress your nervous system's under. It is about how long your body has been on alert. It is, about how times you have tried to fix your skin without giving your skin the time it needs to heal. Your skin needs time to recover from all the things you have done to it. That is why treating acne as a skin problem does not work for a long time.. That is why getting better often means the acne is not completely gone but it is under control, with acne. When we take care of our health our skin usually gets better. This happens when we get rest set boundaries for ourselves and stick to a routine that does not change too much. We also need to avoid doing things that're too extreme. Our skin does not get better away. It does not get better perfectly.. It gets better over time. The redness and swelling in our skin start to go. Our skin heals faster. It also reacts less to things that normally bother it. Mental health is important, for our skin. When mental health is supported through rest and boundaries and predictable routines and fewer extremes our skin often responds to this. This is also the case the way around. When skincare is helpful and does not feel harsh when the products do not dry out your skin or cause pain or require you to be doing something to your skin the body feels better. You stop waiting for your skin to react badly.. This change, in skincare is more important than it seems. Skincare that is supportive makes a difference. This does not mean that acne is all, in your head.. It does not mean that your mindset alone can make your skin clear. It means that your skin and your mental health are talking to each other whether you think about it or not. Your skin and your mental health have a connection. This connection is always there even if you do not realize it. Your skin and your mental health are connected in a way that affects each other. Real progress happens when people respect that relationship. It is very important that we respect the relationship. When we do that real progress can happen with the relationship. These routines seem to be good for acne because they take care of the skin barrier. They do not hurt the skin barrier. It is like being consistent but not too strict. It is like giving your skin the time it needs and being kind to yourself, at the time. Giving your skin time and giving yourself some grace is a thing to do. At Banu we think that taking care of acne is not about fixing the pimples you can see. It should make things easier for your skin not harder. Because having skin is not just about the things you put on your face. It is about making your skin and your whole body feel safe and calm. Clearer skin is, about creating an environment where your skin and your nervous system do not feel like they are always being bothered. At Banu we believe that acne care should help your skin and your nervous system feel better that is why we do what we do at Banu. Acne may show up on the surface, but it doesn’t live there alone. And neither does healing.
-
 read more
read moreHow to Know If Your Skincare Routine Is Actually Working (and What to Do If It's Not)
Skincare routines are supposed to make things simpler. They promise clearer skin, fewer surprises, and a sense that you're doing something supportive — especially when breakouts feel unpredictable. We build them carefully: a cleanser we trust, a treatment we stick with, a rhythm we hope will carry us forward if we stay consistent.
-
 read more
read moreLifestyle Triggers You Might Be Missing When It Comes to Acne: Sleep, Stress, Seasonal Shifts, and Skin
Image Credit: InstagramJanuary skin can feel somewhat confusing to all of us, acne haver or not. Dry one day, congested the next — calm for a week, and then all of a sudden, reactive again. This isn't your skin being unpredictable — it's your body responding to real, everyday shifts. Cold weather, indoor heat, inconsistent sleep, mental load — none of these are "bad habits" — they're normal parts of life, and guess what? Your skin feels them, too. So what's actually going on — and what can you do about it? Let's talk about what's happening and what actually helps. What Your Skin Is Going Through Your skin barrier is working more because of the weather Cold outdoor air and dry indoor heat pull moisture from the skin, weakening the barrier that keeps hydration in and irritants out. When that barrier is compromised, skin loses water faster and becomes more reactive. To compensate, it may produce more oil — which can lead to clogged pores and breakouts, even if your skin feels dry. Your recovery window is shorter Sleep disruption is common in January. Early mornings, late nights, and routine resets all affect how well skin can repair itself. Less repair time means inflammation sticks around longer and blemishes don't resolve as quickly as in warmer months. Your nervous system is a little more activated Mental and emotional load shows up on the skin. Elevated cortisol can increase oil production and inflammation, making skin feel more reactive even if nothing in your routine has changed. Here's What You Can Do Protect your barrier before chasing results When skin feels off, the instinct is to exfoliate or "clear things out." In winter, that often backfires. Instead, prioritize hydration, gentle cleansing, and fewer active-heavy steps. Think support first, correction second. Treat selectively — not everywhere When a blemish appears, it doesn't mean your entire face needs intervention. Spot-level care helps prevent unnecessary irritation and keeps the rest of your skin stable. Work with your sleep, not against it You don't need perfect sleep to support your skin. On nights when rest is limited, simplify your routine. Cleanse, moisturize, and treat only where needed. Lower the overall load This isn’t just about products — drink water regularly and add moisture to indoor air humidifiers if you can. You should try to take breaks from constant routine changes. Your skin prefers steadiness — especially during seasonal shifts. Slow down resets January doesn't need a full skincare overhaul but you can introduce changes gradually. Keep your base routine familiar and reliable, and adjust one thing at a time to see what works and what doesn't. Use These Products When skin is adjusting, targeted care makes the biggest difference. Banu Skin's Sulfur Spot Treatment is designed to treat individual blemishes without disrupting the rest of your face. Instead of spreading strong actives everywhere, this kind of precise approach helps calm inflammation while keeping the skin barrier intact. Use it when a blemish first appears and on areas that need attention — not your whole face. For overall texture, congestion, or buildup, try Banu Skin's AHA + BHA Resurfacing Serum. It supports gentle exfoliation to help keep pores clear and skin feeling smoother — without overwhelming acne-prone skin. This is especially helpful when seasonal dryness and slower cell turnover make skin feel dull or congested. Use it when skin feels your barrier feels stable enough for a resurfacing step. Remember: It's About Progress, Not Perfection Your skin doesn't reset on January 1st. It carries the effects of weather, sleep, stress, and routine changes and that's perfectly normal. Fluctuations aren't so much failures as they are feedback. When you understand what's happening and respond thoughtfully — through lifestyle choices and targeted care — you give your skin room to rebalance on its own timeline.
-
 read more
read moreTravel Season Is the Worst for Acne — Here's What Actually Helps
Travel has a way of throwing skin off. The air is dry, sleep gets weird, routines fall apart, and suddenly your face doesn't feel like itself. When breakouts show up during a trip or right after, it’s usually not because something stopped working — it’s because your skin is adjusting to a lot at once. What actually helps is keeping things simple. Cleansing well at night, supporting hydration, and not overcorrecting when something pops up. A few steady habits go further than panic-switching products mid-trip. When you focus on support instead of control, skin usually settles faster than you expect.
-
 read more
read moreAcne 101
5 Things I’d Do If I Had to Heal My Hormonal Acne All Over Again
Hormonal acne doesn’t play by the same rules as a random breakout. It’s tied to hormone levels, stress, and how your body moves through everyday life. I’ve been there — and if I had to start the healing journey from scratch, here’s exactly what I’d do.
-
 read more
read moreDiet & Lifestyle
PCOS, Acne, and Acceptance: Real Talk From the banu Community
When your skin keeps breaking out, your period feels unpredictable, or your body is sending signals that just don’t add up, PCOS could be part of the picture. Affecting about 1 in 10 people with ovaries, it’s super common in our community — yet still overlooked far too often. And if you’ve ever researched the best skincare for PCOS acne (you're not alone here), you already know how confusing and overwhelming the answers can sometimes be. The signs don’t always look the same for everyone: irregular or missing periods, higher testosterone levels, ovarian cysts (though not always), blood sugar or insulin resistance, and acne that just won’t seem to clear. The important thing to remember? You don’t need to check every box to be living with PCOS.
-
 read more
read moreAcne 101
How to Support a Friend Who’s Struggling With Their Skin
We all know someone — maybe a friend, coworker, or classmate — navigating adult acne or severe acne. Knowing how to be a supportive friend in a situation like this matters, because a strong support system can make progress feel achievable and their mental health a little easier to handle. First, recognize that acne isn’t the same for everyone, it’s usually deeply personal and individual to their own bodily makeup, hormones, and other factors. Adult acne and severe acne can obviously affect confidence, mood, and how your friend navigates the world. So your role? Offer empathy, not judgment (of course). A few encouraging words or simple check-ins can go a long way toward empowering them on their journey.
-
 read more
read moreAcne 101
Let Your Skin Just…Exist: Embracing Acne Neutrality
We’ve all had those mornings. Your reflection greets you with a fresh breakout, and suddenly every scroll on social media feels like a reminder that perfect skin is still the beauty standard. It’s exhausting. That’s where acne neutrality comes in: a mindset that shifts the focus from chasing perfection to finding balance and progress in your skin journey. Instead of idolizing “clear at all costs” or forcing constant self-love, acne neutrality creates space for something more realistic: acceptance and action. It’s about acknowledging that skin can have texture, spots, or redness and still be healthy. And it’s about protecting your mental health and acne by loosening the grip that social media’s highlight reels have on your self-worth.
-
 read more
read moreAcne 101
Late-Summer Skin Slump? Here’s How to Reset Without Stripping Your Barrier
Late summer skin fatigue is real. Long days in the sun, heavier SPF layers, and sticky city air can leave you with clogged pores, rough texture, or a parched skin barrier. The good news? Transitioning your skincare routine from summer to fall doesn’t have to be a full overhaul — it’s about subtle shifts that help you adapt to the season while keeping your skin balanced.
-
 read more
read moreAcne 101
How to Care for Acne-Prone Skin (Without Overcomplicating It)
Let’s get one thing out of the way: acne-prone skin doesn’t only affect people with oily skin. It can happen with dry skin, sensitive skin, even what looks like “normal” skin. It just means your skin is more likely to break out—and needs a more thoughtful approach to care. Whether you’re navigating hormonal flare-ups, product-triggered breakouts, or just want your skin to chill, this is for you.
-
 read more
read moreAcne 101
Sweat, Sunscreen & Skin Freakouts: Your Official Guide to Summer Breakouts
There’s a reason your skin feels more reactive in the summer — and it’s not just the heat. From sneaky breakout triggers like salty ocean swims and poolside chlorine to the way your skincare routine shifts with the season, acne-prone skin needs a little extra attention right now. Consider this your no-stress guide to keeping things clear, balanced, and beach-day ready.
-
 read more
read moreAcne 101
Body Breakouts Are Definitely a Thing — Here’s How to Manage
Let’s talk about body acne — aka bacne, chest acne, shoulder zits, the whole crew. It shows up without warning, overstays its welcome, and doesn’t care that you have a strappy dress to wear Friday. It’s common, it’s manageable, and it doesn’t mean you’re doing anything wrong.
-
 read more
read moreAcne 101
Why You’re Still Getting Breakouts as an Adult
Your skin grew up. Your zits didn’t. Thought you’d graduate high school and leave breakouts behind? Same. But adult acne didn’t get the memo. It’s showing up more than ever—especially for women in their 20s, 30s, even 40s. And while it might look like the teenage stuff, it usually runs deeper, heals slower, and laughs in the face of your old drugstore spot treatment. So what gives? Let’s break down what’s really going on with adult acne, and how to manage it without spiraling.
-
 read more
read moreAcne 101
Is It Acne or Rosacea? Let’s Break It Down
You’re breaking out — but something feels…off. It’s red, inflamed, maybe a little itchy. Is it acne? Is it rosacea? Is your skin just mad at you? Here’s a quick guide to help you figure out what’s going on before you start spiraling on Reddit. Not every breakout is actually acne. If your skin’s always flushed, your “zits” never get heads, or you’ve got stubborn cheek bumps that laugh in the face of regular acne treatments, it could be rosacea—a chronic skin thing that loves to masquerade as the real deal. The catch? Treating it like acne can make it worse. Knowing the difference means you can actually calm it down instead of accidentally starting beef with your skin barrier.
-
 read more
read moreAcne 101
Breaking Out or Purging? Here’s How to Tell — and What to Do About It
You finally commit to a skincare routine — maybe it's your first dip into a retinoid, or you’re flirting with exfoliating acids — and boom: your face suddenly switches up on you. You’re spiraling. Is it a skin purge? A breakout? Is your barrier about to disown you? Take a breath. This might actually be a good sign. A skin purge happens when actives like retinoids or BHAs speed up cellular turnover and push all the junk (clogged pores, micro-breakouts, bad decisions) to the surface. It’s temporary. It’s annoying. But it can be a turning point if you know how to ride it out.
-
 read more
read moreAcne 101
Cryotherapy for Acne: Is It Worth It? Here’s the Chill Breakdown
Cold plunges. Ice rollers. Cryofacials. The skincare world is deep in its “frozen era,” and cryotherapy has officially entered the acne chat. If you’ve seen videos of skin icing or heard about cryofacials and wondered if there’s any real benefit, here’s what you should know. Cryotherapy won’t replace your acne treatments, but it can definitely support them. The right kind of cold therapy helps calm inflammation, reduce redness, and give your skin a little post-breakout breathing room. Let’s get into how cryotherapy works for acne and where a cryofacial fits into your routine.
-
 read more
read moreAcne 101
Skin Cycling 101: How to Reset Acne-Prone Skin
If your shelf is full of half-used exfoliants and “miracle” products you gave up on, same. Skin cycling offers structure, but in a chill, supportive way that actually respects your skin barrier. This routine keeps things gentle, effective, and sustainable. No more guessing games. It’s not a social media trend. It’s a smarter way to treat acne, support your barrier, and finally get consistent results—especially if your skin is sensitive, acne-prone, or just plain tired. Skin cycling can be adjusted according to your skin type, whether it’s oily, dry, or reactive.
-
 read more
read moreAcne 101
How to Pop a Pimple (If You’re Going to Do It Anyway)
We get it. You know you shouldn't pop that pimple, but here you are, standing in front of the mirror, fingers ready. You’re not alone. And while derms usually say “hands off,” sometimes the urge wins. So — if you’re going to pop it, here’s how to do it with the least damage, and the most control. This is just a guide — not a green light for every pimple, especially deep, cystic acne. When in doubt, skip the squeeze and go for a derm. But if you're dealing with a surface-level whitehead? Keep reading.
-
 read more
read moreDiet & Lifestyle
Easy Acne-Friendly Swaps You Can Make in Your Kitchen
Let’s get one thing clear: food doesn’t cause acne. But your diet can absolutely influence it—especially if you’re already prone to breakouts. Research shows that certain ingredients (especially high-glycemic carbs and dairy) may worsen acne by affecting hormones, oil production, and inflammation. The good news? You don’t have to give up all your favorite foods to see clearer skin. Just a few thoughtful swaps, all of which are part of a healthy diet, can make a real difference over time. These acne-friendly food swaps are designed to reduce triggers—not joy.
-
 read more
read moreDiet & Lifestyle
Clear Skin Starts Within: Hormone-Friendly Habits for Breakout-Prone Skin
If your breakouts show up like clockwork before your period, cluster around your chin or jaw, or get worse when you're stressed or sleep-deprived, there's a good chance hormones are involved. And while prescription treatments can be helpful, they’re not the only option. Disclaimer: These tips can help regulate hormones naturally, but they aren’t a substitute for medical care. If you suspect an underlying hormonal condition like PCOS, always consult a healthcare provider or board-certified dermatologist.
-
 read more
read moreAcne 101
What to Know About Oral Acne Meds (and If They’re Right for You)
Topicals can only do so much, especially when you're dealing with deep, stubborn, or hormonal acne. That’s where oral medications come in. They work internally to tackle oil production, inflammation, and hormone imbalances that topicals can’t always reach. Quick note: This guide is research-backed, but nothing replaces a chat with a board-certified dermatologist.
-
 read more
read moreAcne 101
How We're Setting a New Standard for Acne-Safe Skincare
Ever scanned a label for the magic words “non-comedogenic” only to break out anyway? Same. When I was in the thick of dealing with adult acne, I clung to anything that said “for sensitive skin” or “dermatologist-recommended.” Some were even “non-comedogenic,” which I thought was a sure thing. But the breakouts just wouldn’t quit. Eventually, I realized: there’s no real standard for what makes something truly safe for acne-prone skin.
-
read more
Acne 101
The Ultimate Guide to Fading Acne Marks — and Knowing What You're Dealing With
Clearing a breakout is hard enough. But the dark spots, red marks, and weird texture it leaves behind? That’s a whole other ball game. Whether you’re dealing with dark spots, lingering redness, or actual scarring, knowing what you’re working with helps you treat it faster without wasting your time or money. Consider this your cheat sheet to all things acne marks. Shall we?
-
 read more
read moreAcne 101
Pore-Clogging Ingredients to Watch For (and What to Use Instead)
If your acne-prone skin still feels unpredictable — even when you swear you’re doing everything right — it might be time to zoom in on ingredients. Comedogenic (aka pore-clogging) culprits can hide in everything from your cleanser to your conditioner, quietly clogging things up and making breakouts stick around. Even labels like “non-comedogenic” don’t always mean safe. That’s why it pays to know what ingredients to look for, and what to ditch.
-
 read more
read moreDiet & Lifestyle
Snack Smarter, Glow Harder: Food Swaps for Breakout-Prone Skin
No, food alone won’t cause or cure acne. But if you’ve noticed a connection between what’s on your plate and what’s on your face, you’re probably right. Certain foods can mess with hormones, spike inflammation, and crank up oil production — basically, a recipe for breakouts. The good news? You don’t need to overhaul your entire menu. A few easy swaps can help keep your skin happy and your meals delicious. Here are some skin-friendly ones to start with.
-
 read more
read morePost-Acne
Laser Therapy for Acne Scars: When It’s Time and What to Know
You’ve finally made progress calming your acne — but the scars? Still hanging out. If you’re dealing with the aftermath of breakouts and thinking about laser therapy, you’re not alone. Acne laser treatment has become a go-to option for smoothing skin and supporting visible progress, but timing is everything. Let’s talk through what laser therapy can (and can’t) do for acne scars, and how to know when you’re ready.
-
 read more
read moreAcne 101
Accutane: What to Know Before You Say Yes
If you’ve tried everything for severe acne — topicals, antibiotics, and every OTC spot treatment — and still feel stuck, Accutane might be the next step. But before you commit, it’s key to understand how it works, what the side effects are, and why a board-certified dermatologist is your go-to for guidance. Here’s what to know so you can make an informed, empowered decision.
-
 read more
read moreAcne 101
Derm Visits, Decoded: The Acne Questions That Really Matter
Let’s be honest — trying to figure out your acne on your own can feel like a full-time job. If nothing's clicking or things are getting worse, it might be time to call in a pro. That’s where board-certified dermatologists come in. They’ve seen it all, and they’re here to help you cut through the noise. Come armed with these 8 important questions to get the most out of your visit and start seeing results that actually make sense for your skin.
-
 read more
read moreAcne 101
Tretinoin 101: What It Is + Why It Matters for Acne-Prone Skin
Tretinoin’s one of those skincare essentials you’ve probably heard a lot about — especially if you’ve spent time in skincare forums, derm offices, or TikTok rabbit holes. It’s a topical retinoid derived from vitamin A, and it’s a legit go-to from dermatologists for treating acne, fading dark spots, and boosting collagen production over time. But here’s the catch: not all tretinoin is created equal. And if you’re acne-prone, it’s key to talk to your healthcare provider about getting on an acne-safe version early.
-
 read more
read moreAcne 101
What Sulfur Actually Does for Your Skin (and Why It Belongs in Your Routine)
If you’ve dealt with breakouts longer than you'd like to admit, you’ve probably heard of salicylic acid, benzoyl peroxide, and maybe even retinoids. But sulfur? Underrated. It’s got that old-school pharmacy vibe, but don’t sleep on it — it’s gentle, effective, and kind of a sleeper hit for calming chaos.
-
 read more
read moreAcne 101
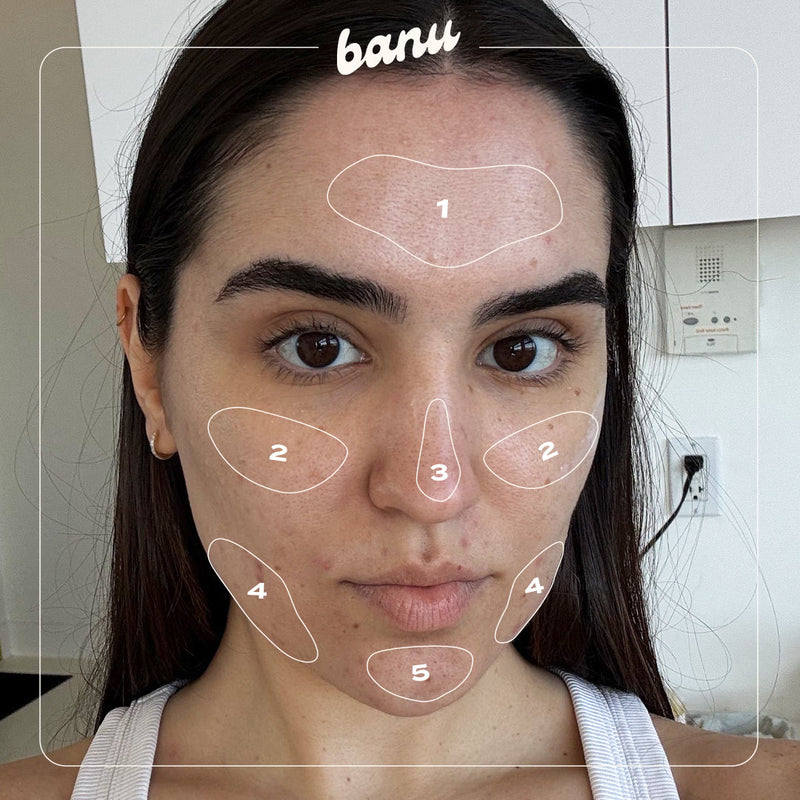
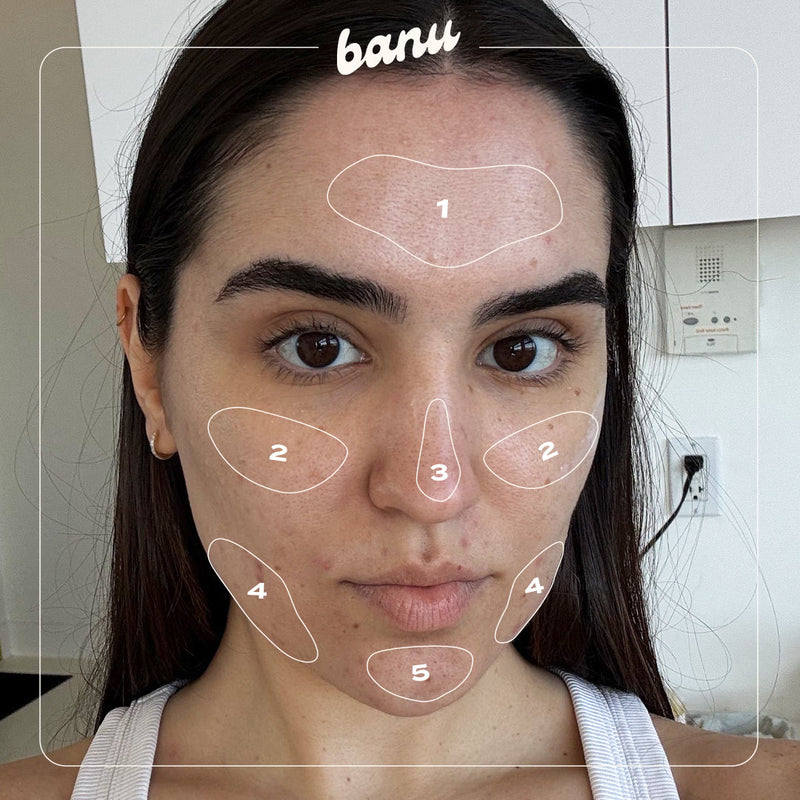
Face Mapping: What The Location of Your Acne is Telling You
If you've ever wondered why it's always your chin, or your forehead, or those same two cheek spots — you're not alone. Face mapping can offer a bit of clarity. Face mapping is an ancient skin-reading practice rooted in Traditional Chinese Medicine. It connects the location of your acne to what's going on internally. Is it exact science? No. But it can be a useful check-in tool when you're navigating your skin journey. Let’s get into what face mapping can (and can’t) tell you—starting with the usual suspects: forehead acne, cheek acne, nose acne, and jawline acne.
-
 read more
read moreAcne 101
Different Types of Acne — and How to Actually Treat Them
Breakouts hit different. Sometimes it's tiny bumps across your forehead. Other times, it’s one deep, angry zit that won’t go away. Knowing your type of acne is key to finding the right acne treatment — because not all breakouts respond the same. Here’s your no-BS guide to the different types of acne, how they show up, and what your skin ~actually~ needs.
-
 read more
read moreAcne 101
What Is Salicylic Acid and Why It Belongs in Your Skincare Routine
Let’s talk about one of the most proven, go-to ingredients in the acne world: salicylic acid. Technically, it’s a beta-hydroxy acid (BHA) — aka an oil-soluble chemical exfoliant that goes deep into pores to clear out dead skin cells and excess oil. Translation? It’s a total MVP for unclogging skin and calming breakouts before they blow up.
-
 read more
read moreAcne 101
PCOS and Acne: Here’s What’s Actually Going On
If your breakouts feel deeper, more painful, and always seem to land around your jawline or chin, there’s a chance it’s more than just your products. For a lot of people, acne is one of the first signs that something internal is off. And one of the biggest culprits? PCOS, aka polycystic ovary syndrome. Let’s break it down.
-
 read more
read moreAcne 101
Non-Comedogenic Isn’t Just a Buzzword — Let’s Break It All Down
If your skin breaks out easily, you’ve probably heard the term non-comedogenic. You’ve also probably Googled “pore-clogging ingredients” at midnight while trying to decode why your skincare might be backfiring. Same tbh. Here’s the deal: if you have acne-prone skin, switching to non-comedogenic products is one of the easiest ways to support your skin — without scrapping your entire routine or falling down a Reddit rabbit hole.
-
 read more
read moreAcne 101
So...Is It a Skin Purge or a Breakout?
You try a new product. A few days later, your face flips out. But before you toss it, pause: is this a breakout, or just a skin purge? And yes, there is a difference. They look similar, but they mean totally different things. One is part of the process. The other? A sign your skincare products might not be it. Let’s make sense of it all so you can move forward with clarity.
-
 read more
read moreAcne 101
Still Breaking Out as an Adult? Here’s Why (and What to Do About It)
Adult acne is SUPER common, and triggers shift with age, stress, hormones, and even the products you use. What worked during your teen years? Probably not cutting it anymore. Let’s break down why you’re still getting acne as an adult — and what you can actually do about it.
-
 read more
read moreAcne 101
Why Am I Suddenly Getting Cystic Acne?
You’re breaking out, and not in the usual way. These spots feel deeper, they hurt, and they stick around way longer than you think they will. Sound familiar? Welcome to the world of cystic acne — frustrating, yes, but manageable with the right approach. Let’s break down why cystic acne shows up and what to do about it (without wrecking your skin in the process).
-
 read more
read moreAcne 101
How to Treat a Pimple Fast (Without Going Overboard)
You’ve got something big coming up...and boom. A pimple. Truly never a good time for them to pop up, unless of course you're dying to get some use out of a new pack of pimple patches. Whether it’s a whitehead, something deeper, or full-on severe acne, breakouts happen. It’s a common skin condition — and yes, there are ways to manage it fast without going overboard. Let’s break it down: why pimples pop up, how to treat them quickly, and what to skip so you don’t make it worse.
-
 read more
read moreAcne 101
Red Light Therapy: Does It Help with Acne?
You’ve tried the spot treatments. You’ve nailed your skincare lineup. Maybe you’ve even cut back on dairy. And now your FYP is full of futuristic red light therapy devices that look like something straight out of a rave promising clearer skin. But can this non-invasive acne treatment really help with one of the most common skin conditions out there? The short answer: Yes, it can. But like most treatments, it’s not a miracle fix — it’s a tool. Here’s what to know about red light therapy (RLT) and how to integrate it into your acne-care routine.
z(it) happens in your inbox